
Total or partial joint replacements for end stage arthritis have been performed with great success for more than 50 years. The most frequently replaced joints are the hip, knee and shoulder. The damaged joints are resurfaced or replaced with implants that provide stable and pain free movement. More than 100.000 knees and 40.000 hips are replaced annually in Turkey. Advances in implant design, materials and instrumentation have led to improved outcomes for patients over the years. Modern joint replacements are expected to last more than 20 years when properly implanted.
Robotic surgery is a recent development in joint replacement leading to increased accuracy during surgery and better recovery. Robotic surgery is not an “experimental” procedure, it has been approved by the F.D.A. in 2008 and over 2 million robotic surgeries have been performed worldwide. Robotic joint replacement is performed in more than 50 countries worldwide and over 2400 scientific publications have been published on the subject, defining its role, advantages and limitations.



Robotic surgery is a recent development in joint replacement leading to increased accuracy during surgery and better recovery. Robotic surgery is not an “experimental” procedure, it has been approved by the F.D.A. in 2008 and over 2 million robotic surgeries have been performed worldwide. Robotic joint replacement is performed in more than 50 countries worldwide and over 2400 scientific publications have been published on the subject, defining its role, advantages and limitations.
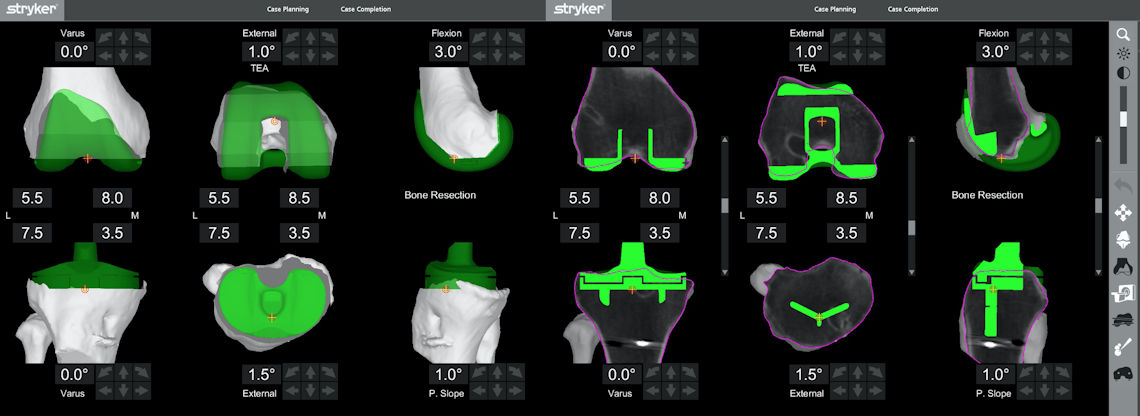
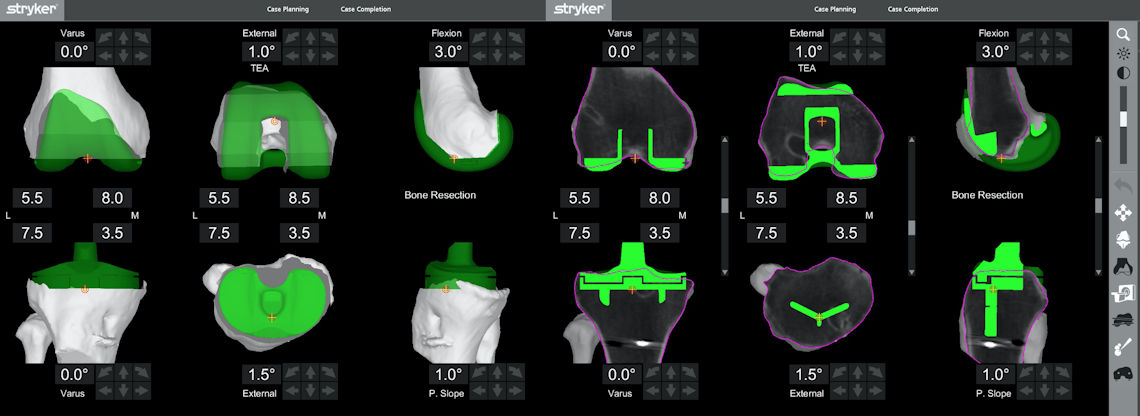
Figure 1: Pre-operative planning is performed with 1 mm accuracy for robotic joint replacement.
What are the advantages of robotic joint replacement?
The implant is placed more accurately during surgery
Robotic systems are accurate to 1 mm and 1 degree, this is three times more accurate than most experienced surgeons. It has clearly been shown that errors of placement more than 3 degrees (the so called “outliers”) lead to decreased in implant life, increased rates of wear and loosening, necessitating early revision surgery. Errors in the size and placement of the implants may lead to residual pain, stiffness and patient dissatisfaction after joint replacement. Malpositioned implants in the hip joint may increase the risk of dislocation, may cause leg length discrepancy and lead to early wear. Robotic joint replacement assures an excellent 3 dimensional placement of the implants during surgery with correct sizing, thus dramatically reducing the risk of these unwanted events.
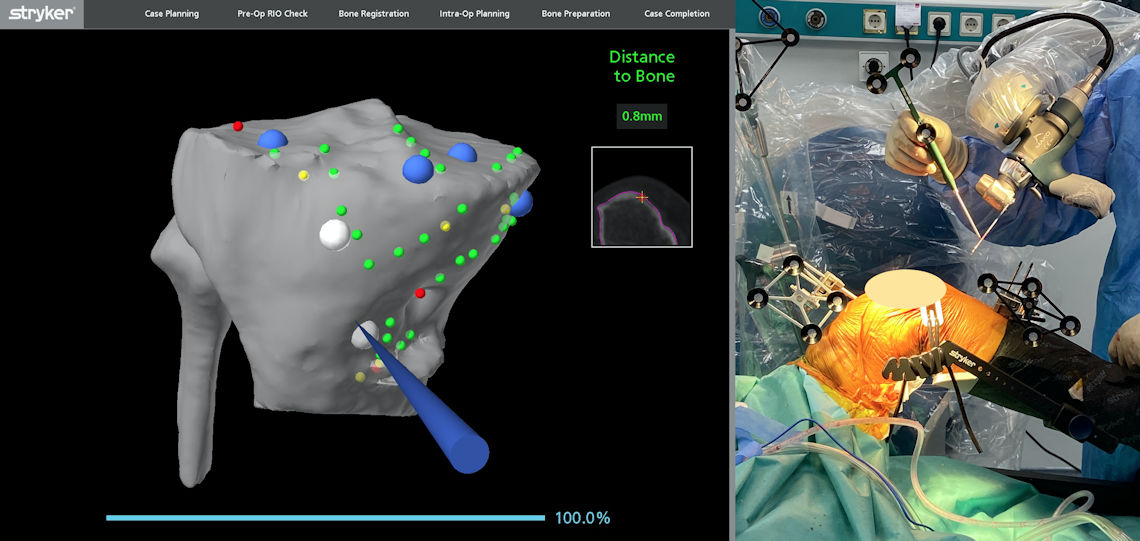
Figure 2: Bone cuts performed with the help of the robotic arm are monitored on the screen.
Excellent soft tissue balance can be achieved
The soft tissue (capsule and ligament) tension and balance is measured and modified in every step of the surgery. Small adjustments during surgery allow a perfectly balanced joint without undue tension on the ligaments causing pain and stiffness after surgery. Excellent stability of the joint is verified with trial implants before implantation of the final prosthetic components. A last check is performed with the implants in place, documenting the final outcome. Soft tissue imbalance is a major cause of patient dissatisfaction after knee replacement. Very lax joints cause a feeling of instability and difficulties in stairs while extremely tight ligaments cause pain, limited range of motion and early wear of the components after knee replacement. Incorrect tension of the soft tissues may cause dislocation after hip replacement. Robotic surgery avoids these problems by achieving excellent soft tissue balance. This balance is helpful during the early recovery phase after surgery, with patients undergoing robotic replacement having an easier rehabilitation.
Figure 3: Assessment of soft tissue balance with the final implants in place. A balanced joint has been attained in every angle of knee range of motion.
The postoperative period is more comfortable
Classical joint replacement surgery requires violation of the medullary canals of the femoral bone and soft tissue releases to achieve ligament balance while robotic surgery requires very little ligament release to achieve a balanced knee. This results in less bleeding and pain following robotic surgery. The avoidance of tourniquet during surgery results in easier recovery of knee motion and less loss of muscle strength. Therefore, the goals of rehabilitation can be achieved earlier with robotic surgery, shortening the length of hospital stay for one day.Patients achieve a more “normal feeling” joint with robotic surgery
Both classical and robotic joint replacements achieve predictable pain relief and functional gains after surgery. Although pain-free, some patients have the feeling that the joint does not feel “normal”, even months after surgery. The “Forgotten Joint Score” is used to quantify a normal feeling joint, with higher scores predicting a forgotten or normal feeling joint. Patients undergoing robotic joint replacement have higher Forgotten Joint Scores compared to classical joint replacement due to the perfect alignment and soft tissue balance attained after surgery.Your implants will last longer
The average life expectancy of a total knee implant is 15-20 years and 20-25 years for a total hip implant. The wear and tear of the implants with daily usage may lead to loosening and may require a second surgery called a revision surgery after a certain time. A variety of factors may influence the longevity of your implant including material quality, surgical technique and patient activity level. The early revision rates of partial knee implants placed using robotic surgery are lower than classical partial knees, meaning robotically placed implants are less likely to be replaced at 5-10 years follow-up. Mid term revision rates of robotic total knee and hip implants are similar to standard surgery. However, it is well known minor errors in implant position and alignment lead to increased rates of failure. Since robotics provide much greater accuracy of implant positioning compared to standard surgery, it is expected that this will result in lower revision rates with robotic surgery at longer term follow-up. It should also be kept in mind that robotics is a constantly evolving technology and the outcomes of early robotic systems may not reflect the current state of the art.Are all robotic systems the same?
A variety of robotic systems are available currently and not all robotic systems are the same. The erly robotic systems were designed as “active robots”, where the role of the surgeon was limited to an “emergency stop switch” once the surgical exposure was made. The robot performed all cuts without any input from the surgeon. Active robotic systems have fallen out of favor due to increased soft tissue complication rates and are no longer used. Semi-active robots, guide the surgeon during the bone cuts and provide visual and tactile feedback to limit the extent of cuts according to the pre-defined plan. However, all bone cuts are performed by the surgeon. MAKO (Stryker) & Navio (Smith & Nephew) systems are examples of semi-active robots and are available for use in Turkey. The final type of robots are called passive robots. Passive robots locate the cutting guides to the desired area but do not provide visual or tactile feedback. All cuts are performed by the surgeon and are not limited by the robotic system. The Rosa (Zimmer Biomet) is an example of a passive robotic system that is available in Turkey.The three robotic systems that are currently in use in Turkey have different properties.
Stryker MAKO system
The pre-operative plan is made on a 3 dimensional model created by a 3-D computed tomography scan of the patient. This model is an exact replica of the patient’s boney anatomy. The patient’s knee is matched to the model created by the software using a procedure called “registration” during surgery. The robot then helps the surgeon execute the pre-operative plan using this real time model. The robotic arm guides the surgeon to the correct angle and location of the cuts and provides visual and tactile feedback during surgery. The robotic arm stops working outside designated areas and prevents the surgeon from making unwanted cuts. Total hip, knee and partial knee systems are available. Soft tissue balance can be adjusted in every step of the procedure.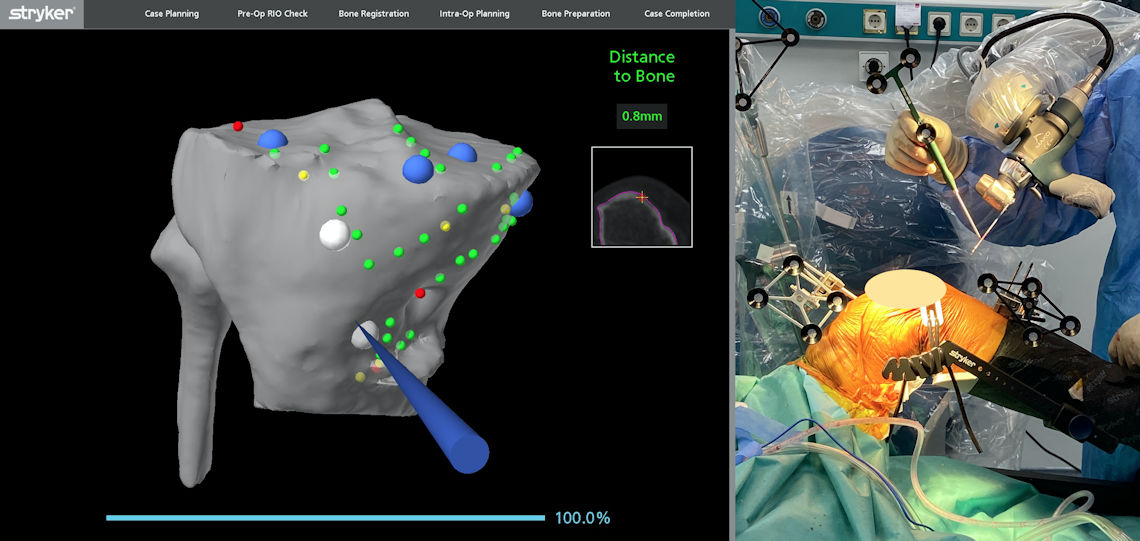
Figure 4: The MAKO robotic system has verifications and security checks at each step of the procedure to avoid erroneous cuts.
Smith & Nephew CORI system
Unlike the MAKO system, the pre-operative plan is made on X-rays and a CT scan is not needed. A virtual model of the joint surfaces is created during surgery, and the bone cuts are performed based on this virtual knee model. The robotic arm stops working outside predefined areas but no tactile feedback is available to the surgeon. Total and partial knee systems are utilized, a total hip navigation system without a robotic arm is available. Soft tissue balance can be measured during surgery.Zimmer Rosa system
The pre-operative plan is made using plain X-rays and the surgeon creates a virtual knee model by registering certain points of the patient’s anatomy during surgery. The robot guides the cutting jig to the intended location, and the cuts are made by the surgeon, no visual or tactile feedback is available. Total and partial knee, total hip and shoulder systems are available.Can every orthopedic surgeon perform robotic joint replacement?
Total joint replacement with standard instrumentation is a part of every orthopedic surgeon’s training. However, robotic surgery requires a specialized training on cadavers and certification process before starting use in patients. Experience with robotics is also important, although robotic systems are accurate from the first case the surgeon performs, the surgery becomes easier and takes less time with surgeon experience. Studies have shown that at least 10 cases are needed before the surgeon becomes comfortable with the robotic system and can use its full potential. Whatever the surgeon experience, robotic systems have built in checks and security systems to prevent unexpected errors.
Figure 5: Your surgeon should be trained and certified for the use of robotic systems. This requires theoretical, saw bone model and cadaver training before using the system on patients.

 TÜRKÇE
TÜRKÇE






